| Mind Games - Recognizing and Handling
Concussions |
| Resources provided by: USA Volleyball and NCAA
Originally Published in: Coaching Volleyball - Provided by: AVCA
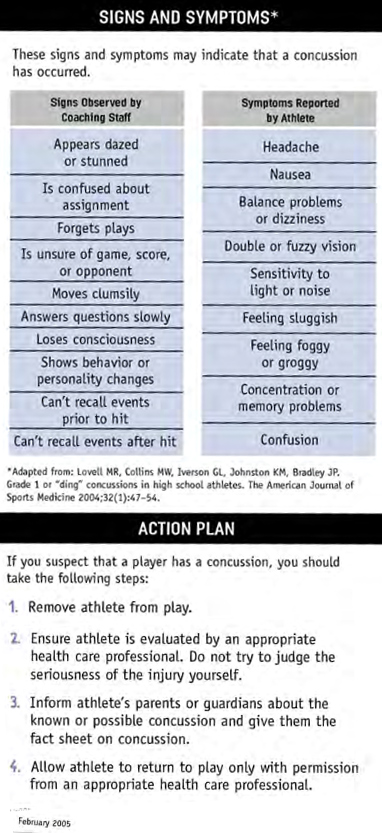
• Concussions can occur in any sport. • A concussion is a brain injury and all are serious. • Most concussions occur without loss of consciousness. • Recognition and proper response to concussions when they first occur can help prevent further injury or even death. What is a concussion? A concussion is a type of traumatic brain injury, caused by a bump, blow or jolt to the head that can change the way your brain normally works. Concussions can also occur from a blow to the body that causes the head to move rapidly back and forth. Even a "ding," "getting your bell rung," or what seems to be a mild bump or blow to the head can be serious. Concussion usually results in functional, rather than structural, disturbances in the brain and as such no abnormality is seen on standard neuroimaging studies. The normal metabolism of the brain is disrupted and shows up in functional deficits and signs and symptoms including but not limited to: headache, ringing in the ears, nausea, disturbed vision, impaired balance, emotional swings, feeling "foggy" or "out of it," slowed reaction times, amnesia, fatigue and possible loss of consciousness. The overwhelming majority of concussion injuries do not involve loss of consciousness. Also, given the variability of signs and symptoms and how different people respond to concussion injury, grading of concussions is no longer part of best practice guidelines. Every concussion should be taken very seriously and managed in a safe, conservative manner. Second Impact Syndrome The still developing brain of the adolescent athlete presents a unique set of challenges in managing concussion injury. The adolescent athlete is more susceptible to a phenomenon known as Second Impact Syndrome. This can occur when an athlete returns to play before all signs and symptoms of a previous concussion have completely resolved and they have gone through an activity progression with no return of signs and symptoms. In this scenario a second trauma occurs, not necessarily a blow to the head or of the same magnitude of the trauma that caused the initial concussion, which sets off a cascade of events resulting in a rapid increase in intra-cranial pressure and disruption of brain stem function. Second Impact Syndrome has a 100% morbidity rate (i.e. transient or long-lasting signs and symptoms) and a 50% mortality rate (i.e. death). Given this possibility, it is imperative that every athlete with a concussion injury be managed in a safe, conservative manner. Return to Play The most important step in caring for a concussion injury is identifying the injury. It is the responsibility of every athlete, coach, parent or other personnel involved with a team to be mindful of the common signs and symptoms of concussion injury discussed above and immediately refer the athlete to a certified athletic trainer for evaluation. Do not wait until the set is over or the match has ended - see the trainer immediately if there is any doubt a concussion has occurred. If an athlete has sustained a concussion injury, current best practice guidelines call for complete physical and mental rest. This means no physical activity, no TV, no cell phone, no computer, nothing, until the athlete is completely asymptomatic. This includes coming to an event to When the athlete is completely asymptomatic they can begin an activity progression. The progression calls for a gradual increase in physical stress while watching for a return of any signs or symptoms. The progression is as follows: Day 1 - 15-minute ride on a stationary bike at a moderate pace (every hotel will likely have a fitness center with a stationary bike and a treadmill) Day 2 - 15-minute ride on a stationary bike at a moderate pace; 2 sets of 15 push-ups, crunches and body weight squats Day 3 - 15-minute jog at a moderate pace; 2 sets of 15 push-ups, crunches and body weight squats Day 4 - controlled volleyball activity (i.e. hitting drills, passing drills, serving, receiving serve - not scrimmaging or match play) Day 5 - if there is no return of signs and symptoms during any step of the activity progression, the athlete should see a certified athletic trainer for evaluation and may be released for full activity. If at any step in the activity progression there is a return of signs and symptoms, the athlete should go back to complete rest until asymptomatic then resume the activity progression one step back from where they experienced a return of signs and symptoms.
|


 watch the team play. Even though the athlete is not playing, the noise level in the convention center or gym and the mental stimulus of following the match will inhibit the athlete's symptoms from resolving.
watch the team play. Even though the athlete is not playing, the noise level in the convention center or gym and the mental stimulus of following the match will inhibit the athlete's symptoms from resolving.